Exclusive AusDoc survey. What you will learn from reading this article:
- Understand what GPs already know about medicinal cannabis
- Explore reasons why GPs do and don’t currently prescribe medicinal cannabis to their patients
- What specific conditions and at what stages GPs would consider medicinal cannabis as part of the overall treatment plan
- Identify key educational needs of GPs and preferred channels for accessing medicinal cannabis information
Doctors are experiencing increased patient demand for medicinal cannabis, but most acknowledge a lack of knowledge about risks and benefits and are unsure how to advise patients, says a 2021 meta-analysis of 21 international articles. Fast-forward to 2023 and not much has changed, according to the results of an AusDoc survey involving more than 240 GPs and specialists across Australia.
Patient mismatch
One thing is clear. Patients are far more interested in medicinal cannabis than their doctors.
In 2016, the Australian Institute of Health and Welfare reported that about 60% of Australian GPs agreed medicinal cannabis should be available on prescription, compared with 85% of the general Australian population.
Unsurprisingly, almost eight out of ten respondents to the AusDoc survey agreed or strongly agreed with the following statement: “Over the past 12-months, more patients are asking me about medicinal cannabis as a treatment option.”
However, doctors are struggling to keep up with patient interest, with only 13% completely confident to answer their questions. Furthermore, four out of ten respondents said they were not at all confident or only slightly confident.
For context, in a 2018 survey of Australian GPs, 61% reported one or more patient enquiries about medicinal cannabis in the previous three months. In addition, most felt their knowledge was inadequate and fewer than a third felt comfortable discussing medicinal cannabis with patients.
Uncertainty about efficacy
According to the AusDoc survey, 44% of respondents overall see medicinal cannabis as a viable treatment alternative for certain groups of patients. This figure is higher for specialists (50%) than for GPs (41%). Notably, about 35% of GPs and 25% of specialists are undecided about the value of medicinal cannabis as a treatment option.
The free text section of the survey showed a high level of disengagement among some doctors. For example: “I don’t recommend it, and if a patient really wants it, they can go looking for themselves,” wrote one respondent.
Little has changed in five years. In the 2018 survey, 44% of GPs agreed they had patients who would benefit from medicinal cannabis, 21% disagreed and just over 34% were undecided or neutral.
Prescribing and referral
Not surprisingly, a minority of respondents to the AusDoc survey said they were current prescribers of medicinal cannabis – 19% of GPs and 9% of specialists. However, 70% of GPs who don’t prescribe will refer their patient to another doctor, often in their own practice.
“Another GP in our practice who is experienced prescriber”
“Patient can self-refer to a GP prescriber they don’t need a referral, I offer a health summary if requested”
Referral rates are much lower for specialists, with 54% saying they would refer their patient to another doctor if they could not prescribe medicinal cannabis.
Few recent adopters
According to the AusDoc survey, few doctors have taken up prescribing in the past year. When asked: “How long have you been prescribing medical cannabis in any form?
- 11% of doctors indicated less than 1 year (9.7% GPs)
- 63% of doctors indicated 1-3 years (64.5% GPs)
- 26% of doctors indicated 3+ years (25.8% GPs)
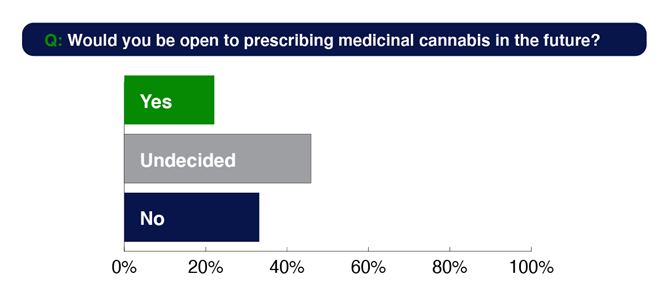
When asked if they would be open to prescribing in future, only 22% are open, 46% are undecided and 33% do not see themselves becoming prescribers.
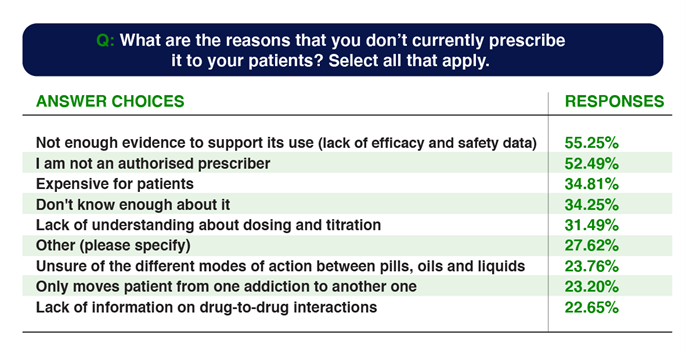
Current prescribing barriers
A lack of knowledge about the risks and benefits is the primary barrier to increased uptake among respondents to the AusDoc survey.
Doctors are also worried about:
- A perceived potential for misuse and addiction.
- A lack of research into the long-term effects of medicinal cannabis, including memory loss, cognitive impairment, and other adverse effects.
- Potential drug-drug interactions.
Barriers to prescribing: 6 verbatim quotes from the AusDoc survey:
- “Not enough evidence to support its use (lack of efficacy and safety data).”
- “It has no supported clinical trials and from observations it does not help improve the condition it is prescribed for.”
- “I am not interested in prescribing it. For me it is an illegal drug causing more problems than good and [there is] no real proof that it works for pain and a big chance of being abused.”
- “Lack of understanding about dosing and titration.”
- “Unsure of the different modes of action between pills and oils.”
6) “It is too expensive.”
Similarly to the AusDoc survey, participants in the 2018 study raised concerns about misuse and dependence. Interestingly, almost half of the GPs who did not want to be able to prescribe cannabis mentioned risk of abuse and dependence.
Current prescribing drivers
According to the AusDoc survey, new options for difficult conditions are the main driver for doctors choosing to prescribe medicinal cannabis. When asked to select reasons for currently prescribing medicinal cannabis:
- 58% of respondents said they had exhausted other options.
- 56% said they were looking for a less addictive alternative to opioids.
- 52% said fewer side effects than current treatment options.
- 48% said patient demand.
- 44% said safer alternative.
In the 2018 study, safety was a major driver, with a significant number of respondents seeing cannabis as less harmful than opioids, benzodiazepines, antidepressants and statins.
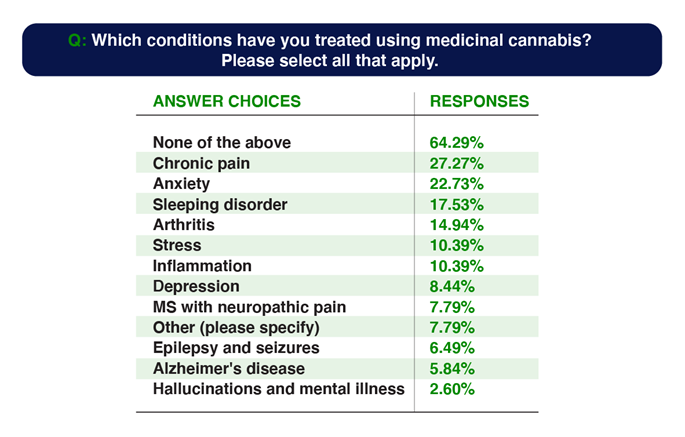
Another driver is that doctors believe medicinal cannabis is a potential treatment for a wide range of conditions. In the AusDoc survey, they ranked these in the following order:
- Chronic pain
- MS with neuropathic pain
- Epilepsy and seizures
- Anxiety
- Sleeping disorder
- Arthritis
- Stress
- Depression
- Alzheimer’s disease
- Hallucinations and mental illness
However when it comes to actual prescribing behaviour, few doctors had actually offered medicinal cannabis to their patients. The answers selected are reflected below.
What doctors say they need
The AusDoc survey respondents indicated that they are hungry to find out more, particularly if information is available on demand to consume in their own time. When asked for their preferred method of learning about medicinal cannabis:
- 66% said they want CPD-accredited online education
- 55% said they want educational webinars (live or on demand)
- 29% want prescribing case studies
- 17% want a visit or online call from a sales representative
Conclusion
Data from the AusDoc survey and other sources indicate increasing consumer interest in medicinal cannabis. However, doctors are not matching this interest with action. They are neither keeping up to date with new evidence nor showing enthusiasm to become prescribers.
A significant challenge to the medicinal cannabis industry is that only 11% of current prescribers in the AusDoc survey had started prescribing in the past year. A more heartening finding is that a high proportion of GP who don’t prescribe medicinal cannabis are willing to refer to another doctor. This shows emerging trust and intertest. Another positive is that respondents to the AusDoc survey are open to finding out more.
And here lies the opportunity for medicinal cannabis marketers. Doctors admit they have a knowledge gap when it comes to medicinal cannabis. Who better to fill that gap than the medicinal cannabis industry?
Sources
- AusDoc Survey: Understanding Doctor insights and behaviours in the use of Medicinal Cannabis (May 2023), n = 241 (all MED’s)
- Rønne ST et al; Physicians’ experiences, attitudes, and beliefs towards medical cannabis: a systematic literature review. BMC Fam Pract. 2021
- Karanges EA et al; Knowledge and attitudes of Australian general practitioners towards medicinal cannabis: a cross-sectional survey. BMJ Open. 2018. https://bmjopen.bmj.com/content/8/7/e022101
- Australian Institute of Health and Welfare (AIHW). National Drug Strategy Household Survey 2016: Detailed findings. Drug Statistics Series No. 31. 2017; https://www.aihw.gov.au/getmedia/15db8c15-7062-4cde-bfa4-3c2079f30af3/21028.pdf.aspx?inline=true (accessed Nov 2017)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8532330/#:~:text=Attitudes%20and%20beliefs%3A%2086%25%20thought,to%20prescribe%20an%20oral%20form